An Overview of Radiation Technology
Radiation Oncology is by its nature a technology-driven medical specialty. We have seen the rapid and exciting development of new radiation technologies that have advanced our field and allowed for more effective cancer care while minimizing short-term and long-term side effects. Presently TIROG doctors have access to the most state-of-the-art radiation equipment and technologies in the world. The technology behind radiation therapy is complex and for some patients there may beadvantages of one technology over another. Since not every hospital location has every treatment modality, our physicians may refer you to another center where the technology may be best suited to your case. Because of our extensive network of treatment facilities, TIROG physicians are able to provide you individualized radiation treatment best suited to your care. Some of the specific techologies available to TIROG physicians include:
CyberKnife
 TIROG physicians have access to an Accuray Cyberknife at the Seattle Radiosurgery Center, the only CyberKnife in the Seattle metropolitan area. The CyberKnife is the world's first and only robotic radiosurgery system. The CyberKnife can allow for radiosurgery treatment throughout the body. This can be particularly useful for inoperable or surgically complex tumors. One of the revolutionary advances in CyberKnife treatment lies in the ability to take real-time x-ray images of the treated area and adapt the treatment in real-time. Often, your physician will have three gold 'seeds' or beads placed in or near a tumor. The machine can see these beads move (for example when you are breathing), and the robotic arm can compensate for this motion, moving with you. This allows for precise radiation treatment in moving tumors, such as lung tumors or prostate cancer. For more information, please see http://www.swedish.org/services/radiosurgery-center.
TIROG physicians have access to an Accuray Cyberknife at the Seattle Radiosurgery Center, the only CyberKnife in the Seattle metropolitan area. The CyberKnife is the world's first and only robotic radiosurgery system. The CyberKnife can allow for radiosurgery treatment throughout the body. This can be particularly useful for inoperable or surgically complex tumors. One of the revolutionary advances in CyberKnife treatment lies in the ability to take real-time x-ray images of the treated area and adapt the treatment in real-time. Often, your physician will have three gold 'seeds' or beads placed in or near a tumor. The machine can see these beads move (for example when you are breathing), and the robotic arm can compensate for this motion, moving with you. This allows for precise radiation treatment in moving tumors, such as lung tumors or prostate cancer. For more information, please see http://www.swedish.org/services/radiosurgery-center.
Gamma Knife
 Also located at the Seattle Radiosurgery Center, the Gamma Knife Icon is the most recent and most advanced Gamma Knife unit in production. Built by Eleckta, the Gamma Knife allows unmatched precision in treating brain tumors. The Gamma Knife has been in use worldwide for over 30 years and has treated hundreds of thousands of patients. It uses 201 Cobalt-60 radiation sources housed in a highly sophisticated enclosure to direct a very precise set of beams to pinpoint accuracy. Usually, a rigid metal frame must be used to prevent even the slightest patient motion during treatment. All 201 beams converge on a pinpoint area, which can be treated to a very high dose while sparing nearby adjacent brain tissue. The Gamma Knife can be used not only to treat cancer, it can be used to treat noncancerous conditions including arteriovenous malformations, benign tumors, trigeminal neuralgia, and essential tremor. Of note, the Seattle Radiosurgery Center is one of the only locations in the U.S. where both a Gamma Knife and CyberKnife are housed under one roof. This allows TIROG physicians the flexibility to use the treatment tool best suited for your individual care.
Also located at the Seattle Radiosurgery Center, the Gamma Knife Icon is the most recent and most advanced Gamma Knife unit in production. Built by Eleckta, the Gamma Knife allows unmatched precision in treating brain tumors. The Gamma Knife has been in use worldwide for over 30 years and has treated hundreds of thousands of patients. It uses 201 Cobalt-60 radiation sources housed in a highly sophisticated enclosure to direct a very precise set of beams to pinpoint accuracy. Usually, a rigid metal frame must be used to prevent even the slightest patient motion during treatment. All 201 beams converge on a pinpoint area, which can be treated to a very high dose while sparing nearby adjacent brain tissue. The Gamma Knife can be used not only to treat cancer, it can be used to treat noncancerous conditions including arteriovenous malformations, benign tumors, trigeminal neuralgia, and essential tremor. Of note, the Seattle Radiosurgery Center is one of the only locations in the U.S. where both a Gamma Knife and CyberKnife are housed under one roof. This allows TIROG physicians the flexibility to use the treatment tool best suited for your individual care.
Prostate Brachytherapy
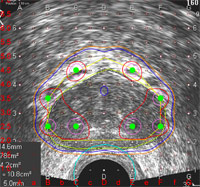 The Seattle Prostate Institute (SPI)pioneered the use of prostate brachytherapy – the technique of delivering radiation 'seeds' to the prostate under ultrasound guidance. The institute was established in 1997 by our physicians who had developed this technology in the mid 1980s here in Seattle. SPI physicians have performed more than 10,000 prostate implants. Almost half of these patients have come from other states and countries in order to benefit from our expertise. Prostate brachytherapy has taken off as a preferred method of treating low-risk prostate cancer, in part due to the robust long term data that we have published showing high cure rates and low toxicity. Physicians, residents, and other health professionals attend the Seattle Prostate Institute educational courses and our annual conference. SPI physicians have maintained their leadership role through these lectures, our research, and by providing ongoing assistance to physicians around the country with our remote dosimetry services. The Seattle Prostate Institute is the prostate cancer 'arm' of TIROG.
The Seattle Prostate Institute (SPI)pioneered the use of prostate brachytherapy – the technique of delivering radiation 'seeds' to the prostate under ultrasound guidance. The institute was established in 1997 by our physicians who had developed this technology in the mid 1980s here in Seattle. SPI physicians have performed more than 10,000 prostate implants. Almost half of these patients have come from other states and countries in order to benefit from our expertise. Prostate brachytherapy has taken off as a preferred method of treating low-risk prostate cancer, in part due to the robust long term data that we have published showing high cure rates and low toxicity. Physicians, residents, and other health professionals attend the Seattle Prostate Institute educational courses and our annual conference. SPI physicians have maintained their leadership role through these lectures, our research, and by providing ongoing assistance to physicians around the country with our remote dosimetry services. The Seattle Prostate Institute is the prostate cancer 'arm' of TIROG.
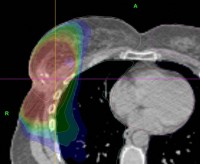
Arc-Based Radiation Therapy
 External beam radiation machines have been undergoing steady modification and improvements. One of the most recent exciting advances is Eleckta's VMAT – volumetric arc therapy. Rather than using fixed beam angles to treat a tumor, VMAT allows the machine to swing in an arc, offering more precision and control of the radiation dose. Presently this technology is offered at several of our radiation centers. We were one of the very first groups of physicians to use VMAT in the United States and are involved with research and training for Eleckta's new technologies.
External beam radiation machines have been undergoing steady modification and improvements. One of the most recent exciting advances is Eleckta's VMAT – volumetric arc therapy. Rather than using fixed beam angles to treat a tumor, VMAT allows the machine to swing in an arc, offering more precision and control of the radiation dose. Presently this technology is offered at several of our radiation centers. We were one of the very first groups of physicians to use VMAT in the United States and are involved with research and training for Eleckta's new technologies.
Calypso 4D Localization
 Calypso was pioneered by radiation oncologists in Seattle, particularly from TIROG, to improve the localization of a tumor within the body. The technology is now FDA approved and Calypso units are being sold worldwide. Because of our role in its development, TIROG physicians were the first in the world to use this technology and have therefore extensive experience with Calypso. Called 'GPS for the body', Calypso uses three implanted RFID (Radio-frequency Identification) beacons to track a tumor real-time. The beacons are inserted into or near the tumor prior to beginning external beam radiation therapy. During treatment, a specialized detector is placed over the patient that allow detection of even very small movement. This allows the radiation therapy staff to stop or re-position a patient in order to ensure the most precise and accurate treatment.
Calypso was pioneered by radiation oncologists in Seattle, particularly from TIROG, to improve the localization of a tumor within the body. The technology is now FDA approved and Calypso units are being sold worldwide. Because of our role in its development, TIROG physicians were the first in the world to use this technology and have therefore extensive experience with Calypso. Called 'GPS for the body', Calypso uses three implanted RFID (Radio-frequency Identification) beacons to track a tumor real-time. The beacons are inserted into or near the tumor prior to beginning external beam radiation therapy. During treatment, a specialized detector is placed over the patient that allow detection of even very small movement. This allows the radiation therapy staff to stop or re-position a patient in order to ensure the most precise and accurate treatment.
Intensity Modulated Radiotherapy (IMRT) and
Image Guided Radiotherapy (IGRT)
 IGRT and IMRT are very significant advances in the field of external beam radiation therapy. Developed and refined over the past several years, they have now become much more widely adopted by radiation oncologists nationally and internationally. Standard radiation in the modern era is called '3D conformal radiation'. With 3D treatment, multiple beams are used and shaped to optimally treat a tumor while sparing normal tissue. However IMRT represents an advance because the amount of radiation delivered across any particular beam can vary. This is achieved by rapidly sliding 'multileaf collimators' which enter and exit the beam quickly, changing the characteristics of the beam profile. Combined with multiple radiation fields, it offers more flexibility in treating tumors and protecting normal organs. IGRT refers to image guided radiation therapy. With IGRT, tumor localization is used which gives instant feedback to the radiation therapy team and allows for refinement of patient positioning. For example, some modern linear accelerators use an on-board CT scanner, others use diagnostic x-rays combined with implantable gold markers (called fiducials). Calypso (described above) is a type of IGRT. IGRT and IMRT represent a significant advance in many cases but are not always indicated or advantageous. Your physician can help explain the details of treatment delivery and the best techology available. TIROG is a leader in IGRT and IMRT technologies. We teach regular IGRT educational courses which are attending by radiation oncologists worldwide. IMRT and IGRT are now available at all of the radiation treatment locations where TIROG physicians practice.
IGRT and IMRT are very significant advances in the field of external beam radiation therapy. Developed and refined over the past several years, they have now become much more widely adopted by radiation oncologists nationally and internationally. Standard radiation in the modern era is called '3D conformal radiation'. With 3D treatment, multiple beams are used and shaped to optimally treat a tumor while sparing normal tissue. However IMRT represents an advance because the amount of radiation delivered across any particular beam can vary. This is achieved by rapidly sliding 'multileaf collimators' which enter and exit the beam quickly, changing the characteristics of the beam profile. Combined with multiple radiation fields, it offers more flexibility in treating tumors and protecting normal organs. IGRT refers to image guided radiation therapy. With IGRT, tumor localization is used which gives instant feedback to the radiation therapy team and allows for refinement of patient positioning. For example, some modern linear accelerators use an on-board CT scanner, others use diagnostic x-rays combined with implantable gold markers (called fiducials). Calypso (described above) is a type of IGRT. IGRT and IMRT represent a significant advance in many cases but are not always indicated or advantageous. Your physician can help explain the details of treatment delivery and the best techology available. TIROG is a leader in IGRT and IMRT technologies. We teach regular IGRT educational courses which are attending by radiation oncologists worldwide. IMRT and IGRT are now available at all of the radiation treatment locations where TIROG physicians practice.
Accelerated Partial Breast Irradiation
 Accelerated Partial Breast Irradiation (APBI) is not a technology per se, but a radiation technique which has been of great interest to both radiation oncologists and patients. Typical breast irradiation occurs over 6-1/2 weeks, allowing for time for normal tissue to heal and repair. With APBI, only the tumor bed is targeted and the treatment is delivered twice a day for just one week. Often this is a great convenience to patients. A large national randomized trial is being conducted (NSABP-B39) comparing this approach to standard full-breast radiation. Since the complete results of this trial have not yet been reported, we generally treat only very favorable tumors with this approach. Not all breast cancers are suitable for treatment with IGRT and it is important to have a detailed discussion with your radiation oncologist regarding the pros and cons of this approach. During your consultation, the TIROG physician can update you on the latest data in regards to APBI, and determine if you might be a candidate for this novel approach.
Accelerated Partial Breast Irradiation (APBI) is not a technology per se, but a radiation technique which has been of great interest to both radiation oncologists and patients. Typical breast irradiation occurs over 6-1/2 weeks, allowing for time for normal tissue to heal and repair. With APBI, only the tumor bed is targeted and the treatment is delivered twice a day for just one week. Often this is a great convenience to patients. A large national randomized trial is being conducted (NSABP-B39) comparing this approach to standard full-breast radiation. Since the complete results of this trial have not yet been reported, we generally treat only very favorable tumors with this approach. Not all breast cancers are suitable for treatment with IGRT and it is important to have a detailed discussion with your radiation oncologist regarding the pros and cons of this approach. During your consultation, the TIROG physician can update you on the latest data in regards to APBI, and determine if you might be a candidate for this novel approach.
Radionucleides - Pluvicto, Lutathera
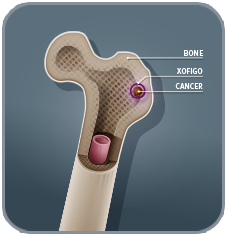 The treatment options for cancer patients continue to expand. We have been at the forefront of radioligand therapy and have an active program for several isotopes. Pluvicto is a radioligand for PSMA+ metastatic prostate cancer. It targets a biomarker called PSMA, which is present on many prostate cancer cells. This means it is designed to find and attack PSMA+ cells in the body, when prostate cancer has spread outside the prostate gland. Similarly, Lutathera (Lutetium Lu 177 dotatate) is an injection targeting neuroendocrine tumors. These tumors often secrete extra amounts of hormones that may cause symptoms such as flushing and diarrhea. Lutathera can deliver targeted radiation to these neuroendocrine tumors through an intravenous route. Several new isotopes are in development for patients with metastatic cancers and we are committed to help these transition from the bench to bedside.
The treatment options for cancer patients continue to expand. We have been at the forefront of radioligand therapy and have an active program for several isotopes. Pluvicto is a radioligand for PSMA+ metastatic prostate cancer. It targets a biomarker called PSMA, which is present on many prostate cancer cells. This means it is designed to find and attack PSMA+ cells in the body, when prostate cancer has spread outside the prostate gland. Similarly, Lutathera (Lutetium Lu 177 dotatate) is an injection targeting neuroendocrine tumors. These tumors often secrete extra amounts of hormones that may cause symptoms such as flushing and diarrhea. Lutathera can deliver targeted radiation to these neuroendocrine tumors through an intravenous route. Several new isotopes are in development for patients with metastatic cancers and we are committed to help these transition from the bench to bedside.
Breast Microseed Treatment
Breast Microseed Treatment is a relatively novel method of radiation therapy for women with early-stage breast cancer following a lumpectomy. Using brachytherapy, Breast Microseed Treatment involves the precise placement of radioactive seeds in the breast that slowly release the prescribed dose safely over time. Microseed™ radiation sources are implanted in and around the area where the tumor was removed, which is typically the area where cancer might recur. We provide this treatment at Swedish Cancer Institute at the First Hill Campus.
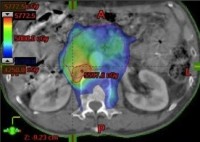
Yittrium-90 Theraspheres
 Yittrium-90 Microspheres Theraspheres are glass microspheres containing a radioactive isotope called Yittrium-90. They are designed to deliver radiation directly to a tumor and are most often used to treat tumors in the liver, such as hepatocellular carcinoma. The spheres are delivered through transfemoral catheterization of the hepatic artery. The spheres then penetrate and lodge within the tumor arteriolar capillaries, where they emit lethal beta radiation that is localized to the area of the tumor. This can be used for patients with unresectable hepatocellular carcinoma, and is particularly useful in patients who have larger tumor size, multifocal tumors, or have developed a recurrence following other treatment techniques such as TACE.
Yittrium-90 Microspheres Theraspheres are glass microspheres containing a radioactive isotope called Yittrium-90. They are designed to deliver radiation directly to a tumor and are most often used to treat tumors in the liver, such as hepatocellular carcinoma. The spheres are delivered through transfemoral catheterization of the hepatic artery. The spheres then penetrate and lodge within the tumor arteriolar capillaries, where they emit lethal beta radiation that is localized to the area of the tumor. This can be used for patients with unresectable hepatocellular carcinoma, and is particularly useful in patients who have larger tumor size, multifocal tumors, or have developed a recurrence following other treatment techniques such as TACE.